by Hamilton E. Davis
In my last post, we took an overview of Bruce Hamory’s 144-page recommendations to the Green Mountain Care Board on how to recast Vermont’s 14-unit hospital system. In the process, we cast aspersions on that effort—overly broad, impossibly expensive, filled with internal contradictions, and just too complicated to execute in the real world. That took us through page 12 of the report.
The job today is to parse the evidence in the remaining 132 pages. It’s critically important: The GMCB is taking a wrecking ball to the system, and it has to be reined in this fall. If no one can do that, Vermonters will pay the price in an existential threat to not just their health care system, but to the state economy itself.
The first thing to understand is that there are two Hamory reports to the GMBC, not one. The second thing is that the second report contradicts the first. In my view that demonstrates that Hamory’s latter report, the detailed 144-page map for a rebuilt Vermont doctor/hospital system, is a total sham. I suggested in my previous post that Hamory’s performance resulted not from his expertise, but from his ability to read his client—he can see that Owen Foster, the GMBC chairperson, is determined to take down the UVM Health Network. Of course, that is just speculation; teasing out motivation is always chancy. So, let’s look at the hard evidence:
Look at what Hamory concluded from his work on the Board’s Sustainability Project, launched in 2019. The basis for that work was very broad—seven national-class health policy consultants, whose work flowed into the Board beginning on Oct. 27, 2021 and concluding in February of 2022. Hamory’s presentation in February opened like this:
PROBLEM STATEMENT FOR SMALL VERMONT HOSPITALS
Eight of 14 Vermont hospitals have Operating revenue ranging from -0.9% to – 12.8% (GMCB)
The Proportion of Total hospital revenue (ED and Inpatient) in these facilities from potentially avoidable admissions ranges from 21.5% - 37%. (Mathematica)
Average daily census (ADC) in Small Vermont hospitals averages 15 inpatients. (GMCB)
Analysis of bed needs for 2026 in Vermont hospitals showed reduction of 153 beds for hospitals other than UVM (BRG)
Model of basic support personnel costs for a 20 bed hospital with ADC of 5 inpatients and a skeletal ED staff yields total cost of $2,200,000.00 This does not include any medical support for ED, OR or inpatient care. (OW analysis) (OW means Oliver Wyman so Hamory is quoting his own work)
How can Health Services be provided to these communities understanding these and other constraints?
The answer to that is they can’t. A fair reading of Hamory’s 2022 report is that he is broadly endorsing the work of his professional colleagues, but he didn’t mention a word of that in his fall 2024 report. Look at what he says there:
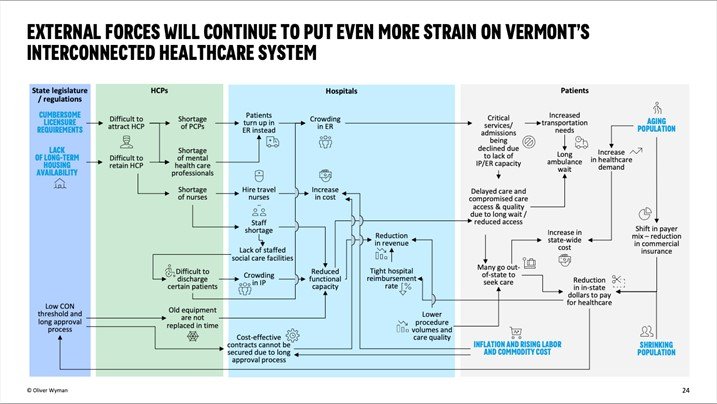
Focus on the numbers on the far right: The top one in black is 2.4 percent. That is what Gifford Hospital, a 25-bed facility in Randolph, would achieve as a margin in 2028. The remaining 13 hospitals are shown drowning in red ink, ranging from 1.5 percent to 14.4 percent. Hamory doesn’t identify which number goes with each hospital. It would be possible to suss that out by tying the percentage loss to each specific hospital to the budget orders, but it would be a waste of time, which you can infer from the Hamory diagram below:
There may be people out there who would spend a fun afternoon wandering through that maze, but I’m not one of them. The central point is not the map—it’s the fact that the whole Hamory document is DOA, dead on arrival, and the real question is what the hospitals themselves and the Legislature decide to do about it. Still, the state is paying for this report, and Vermonters deserve to get at least some sense of what they bought.
The overarching problem with Hamory’s 144-page report is that it ignores the reality of what’s happening on the ground today. For example, Hamory lays out his recommendations for each hospital in the state, but he ignores how the whole eastern part of the state gets its most sophisticated care from the Dartmouth-Hitchcock Medical Center in nearby New Hampshire. He also ignores the extent to which small and very small hospitals rely on the tertiary care from the 500-bed academic medical center hospital in Burlington.
Take Brattleboro Memorial Hospital for example. The southeast anchor for the system, Brattleboro has just 47 staffed beds—far too small for a modern full-service facility. Yet, Hamory recommends trying to make it a center for orthopedics, including spine surgery which belongs in tertiary centers. And Dartmouth sits just an hour’s drive north.
That kind of just plain bad analysis taints Hamory’s analysis of hospitals in Newport, St. Johnsbury, White River, Randolph, and Grace Cottage in the east, and St. Albans in the UVM Network patient shed. But does it matter?
Among the official responses to the Hamory study, two stand out. The first came earlier this week from Jenny Samuelson, the Secretary of the Agency of Human Services. She sounded polite but underwhelmed:
I want to reassure Vermonters that any solutions we identify will be thoroughly evaluated, she wrote. They will be both fiscally sound and operationally feasible. We will make sure our next steps improve patient access, quality, and affordability for Vermonters, and make sure that our local community health systems are strong and viable into the future.
Mike Del Trecco, the CEO of the Vermont Hospital Association, by contrast, excoriated the whole Hamory effort:
Many of the recommendations are deeply concerning. Cutting, consolidating and closing services across Vermont will have devastating impacts to our patients and communities. The report essentially calls for the closure of four hospitals, creating healthcare deserts in rural regions. It has no compassion or acknowledgment for the damaging healthcare outcomes that will result from delayed care and long drives in emergency situations or the ripple effects on community healthcare and the local economy. It calls for the consolidation of orthopedics to northern and southern Vermont, leaving Vermonters along the spine of the Green Mountains with nowhere to go but to drive hours or leave the state.
It suggests women should have no choice but to give birth in yet-to-be-built stand-alone birthing centers with no assurances of higher-level care in an emergency. And the list goes on.
Del Trecco did not return a call asking whether he would recommend that any of his member hospitals challenge the budget orders entered by the GMCB. Nevertheless, that is the existential question facing the decision-makers in the state’s hospitals. Resist an ignorant, dangerous board or what—abandon their missions, just die? This post is going up on October 18. Unchallenged, the Board’s orders lock in on Oct. 31, 13 days out…
The decision is critical for many of them, but by orders of magnitude it is most apposite for the UVM Health Networks hospitals in Burlington, Berlin and Middlebury. Since the Scott administration took office in 2017, its Green Mountain Care Board has drained hundreds of millions of dollars from the UVM facilities, an effort in service to the idea that the only way to keep private insurance rates closer to affordable is to get all the money they can out of UVM.
The question, therefore, is the one I posed for the Network in a recent post, Leader or Doormat: Will the University of Vermont’s Health Network be the leader of Vermont’s healthcare delivery system, or a doormat for a failing state government and regulatory system? To lead, the UVM Network would have to appeal the budget decision in the next 13 days. So far they have been moving far too slowly to get that done. The question remains open for another couple of weeks, but there hasn’t been a hint out of Sunny Eappen, his Board, or his senior management about whether they’ll just complain or for the first time challenge the Green Mountain Care Board.