by Hamilton E. Davis
The Green Mountain Care Board accepted a staff report Thursday showing that eight of Vermont’s 14 hospitals had exceeded its spending cap for Fiscal Year 2016, which ended last Oct. 1. While the other six facilities came in under budget, they were all smaller facilities.
The hospitals blowing through the cap account for 86 percent of the system’s $2.3 billion total spending for that year. The Board has summoned representatives of the six larger hospitals to appear before it Tuesday to explain the variances from the budgets. Scheduled to testify are the University of Vermont Medical Center, UVM’s sort-of-partner Central Vermont Medical Center in Berlin, Rutland Regional Medical Center, Northeastern Medical Center in St. Johnsbury, and Northwestern Medical Center in St. Albans.
The Board opted to excuse two smaller institutions—North Country Hospital in Newport and Copley in Morrisville. According to Mike Davis, the Board’s finance chief, North Country wasn’t over the cap by much and its compliance with Board guidance has been good over the last few years. And Copley, whose budget was basically a shambles last year and is now under new leadership, rebuilt its budget as of last December and there hasn’t been time enough for those changes to take hold.
On a system-wide basis, according to Davis, the hospitals exceeded the 3.4 percent growth cap by 2.6 percent, which amounted to $60.3 million. That figure did not include a total $10.5 million for the movement of independent doctors into the hospitals. Those doctors were not inside the Board’s regulatory structure, but were nevertheless getting paid for their services by federal and state governments and commercial insurers, so that at least part of the $10 million is a wash—it’s not new money to be paid by Vermonters.
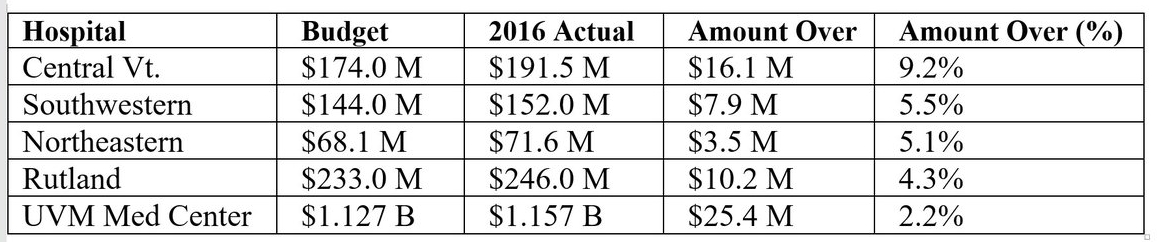
The Actual Numbers
These numbers include the physician transfers, but it doesn’t make a lot of difference. The pattern is clear enough. And what the pattern says is that plain old regulation isn’t strong enough to drive hospital cost inflation into the sustainable range.
The inflation rate that Vermonters can afford to pay each year runs to just over three percent, or even less. And the inflation rate we’ve been living with is north of four percent per year, which isn’t one percent too high, but 33 percent too high.
The three members of the Board (there are two vacancies) did not seem overly concerned about the final numbers for the last fiscal year. Con Hogan, for example, remarked that he felt good about the overall state of the overall state of the Vermont system.
There are at least three reasons for that. One is that the Vermont inflation rate is not yet sustainable, but it is lower than most of the rest of country, which is running at about six. A second is that spending for the first five months of the current fiscal year (FY2017) is tracking closely with the approved budgets; in fact, spending is running below budget by half a percent, whereas it was over by 1.1 percent at the this time last year.
By far the most important reason, in my view, is that Vermont is now embarked on the key to sustainable level reform, which is to shift reimbursement for health care from fee-for-service to capitation, about which more in a moment.
The immediate question, however, is what happens in the short term.
Well, the Board will have to take the 2016 actuals and incorporate them into their determination of the FY 2018 budgets, which will take effect on Oct. 1 of this year. They have some obvious tools at hand. One is to calculate the extent to which the overspending has dropped to the budgeted bottom line, or profit in a non-profit system, and then order the institutions to cut its rates by that amount. That, in fact, is what they have done in the past.
The real solution, however, lies not in more regulation, or tougher or better regulation, but in the move from fee-for-service reimbursement to block financing or capitation. That shift is already underway in the form of the capitation contract now in effect between state Medicaid officials and a four hospital cluster in northwestern Vermont.
UVMMC, Central Vermont, Northwestern and Porter in Middlebury have agreed to deliver care to 31,000 Medicaid patients in that region for a set price per month. Each hospital gets a set payment each month for the target population—and that’s it.
There isn’t any more money.
That is the solution to the cost inflation problem, and the first iteration of the ultimate in reform is now underway in Vermont. The first checks went out for February.
When the GMCB convenes Tuesday, they will spend a whole day listening to reasons, excuses, and rationalizations of all descriptions until their heads spin. Every single dime of inflation will be backed up by perfectly good reasons why it couldn’t be avoided. Vermont hospital CEOs and CFOs have been going through that exercise since the mid-1980s. and they are really good at it.
The fact that shifting reimbursement and reorganizing the delivery system is the only way to cut that knot doesn’t mean that Vermont will actually follow through and do it. The health policy community from one end of the country to the other, and every hospital executive who doesn’t have his or her head under water, knows it is true.
But that judgment doesn’t necessarily extend to our new Gov. Phil Scott, or to the Vermont Legislature, including its left as well as its right wing, or to the Vermont press corps, or to the public at large.
I’ll explore that question in my next post.
####